
Current disability issues and the NDIS
For a deep dive into issues and developments in disability advocacy and the National Disability Insurance Scheme, visit Hayley’s Journal.

Mar 2025: A Call for Change: Hearing Services in Australia
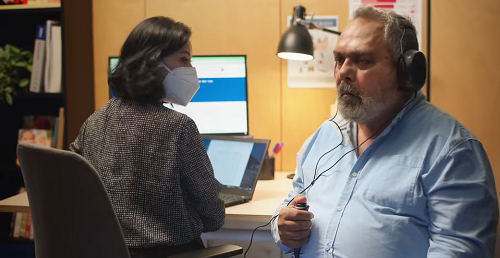
A pressing need for systemic reforms and increased regulation has been revealed in a survey conducted by Deafness Forum Australia that sheds light on the complex landscape of hearing services in the country.
Deafness Forum Australia wanted to capture the experiences of receiving or delivering hearing services in Australia. Our constituents (consumers primarily, but also service providers) were invited to complete an in-depth survey that was distributed through its newsletter and social media posts from November 2024 to January 2025.
The survey asked for detailed information including beliefs, knowledge and personal experiences of receiving or delivering hearing health related services.
Read the complete survey report: use the form here to request your copy of the report.
Consumer Perspectives
The survey uncovered a disconnect between consumer expectations and their experiences with hearing services.
There appears to be confusion among consumers about the roles of audiometrists and audiologists, with some expressing uncertainty about the expertise each profession possesses. This points to a need for better public education about professional roles and where the current system could be enhanced.
Terms like ‘audiology professionals’, ‘audiology profession’ and ‘audiology clinics’, are often used in advertising which can contribute to consumer confusion about the qualifications of different service providers.
We believe that establishing a consistent national standard for both audiologists and audiometrists, supported by strong governance structures and evidence-based data, could help ensure that consumers receive accurate information. This approach aims to empower individuals to make informed decisions about their hearing health care. We are committed to collaborating with all stakeholders to ensure that these improvements are made together, with them, and not for them.
So, back to the results of our survey:
Survey respondents wanted expert guidance on managing their hearing loss but might encounter aggressive sales tactics promoting costly hearing aids.
These consumers expressed a strong desire for:
- Ethical, comprehensive services
- Simplified access to care
- Increased provider awareness of cultural and community-specific needs
Most tellingly, these consumers have a perception that those providing hearing services are primarily salespeople. This view starkly contrasts with how these professionals see themselves.
Provider Insights
On the other hand, respondents who were providers of hearing services voiced their own frustrations with the current system. Some reported feeling caught between their professional ethics and commercial pressures.
“We entered this field to help people, not to meet sales targets,” one audiologist commented anonymously.
These providers called for:
- Reduced commercialism in the industry
- Increased regulation to standardise practices
- Greater transparency in professional qualifications and roles
The Regulation Debate
A key survey finding was the support for regulating audiologists to align with other healthcare professionals. Both consumers and providers see formal regulation as crucial for:
- Defining explicit scopes of practice
- Ensuring accurate use of professional titles
- Enhancing professional recognition and accountability
However, the survey also revealed that regulation alone may not address all the issues affecting the industry, particularly those related to commercialism.
Thoughts on Regulating Audiometrists
The Australian College of Audiology has recommended to its member audiometrists that they, too, should be regulated along with audiologists. Deafness Forum Australia supports this as a medium-term objective, to be addressed once the current investigation into regulating audiologists is concluded.
The Current Landscape
To understand the significance of these findings, it’s important to consider the current state of hearing services in Australia. As of January 2025, the industry operates under a patchwork of partial regulations and self-governing bodies. Hearing services are overseen by:
- Government funding bodies like the Hearing Services Program, NDIS, and Medicare
- Self-regulating professional associations
- Healthcare commissioners in each state or territory
There is no national board under the Australian Health Practitioner Regulation Agency (AHPRA) for hearing service providers. This fragmented system has confused consumers about the qualifications and roles of different providers. Many struggle to differentiate between audiologists, who hold master’s degrees, and audiometrists, who typically have diplomas or certificates.
Adding to the complexity, many hearing-related businesses are owned by companies associated with hearing device manufacturers.
The current regulatory arrangement bears, in our opinion several hallmarks necessitating Government intervention. We need a regulatory framework which generates the greatest net benefit for the community and inspires greater community trust.
The Road Ahead
Based on the survey findings, Deafness Forum Australia has outlined a suite of recommendations for systemic reforms which would both achieve efficiency of the industry and substantially enhance net benefit for community:
- Mandatory Regulation: Implement comprehensive regulation for both audiologists and audiometrists under a national framework.
- Patient-Centred Care: Shift the focus of hearing services from device sales to holistic, individualised care.
- Reduced Commercial Pressure: Develop strategies to mitigate the influence of commercial interests on clinical decision-making.
- Public Education: Launch initiatives to educate the public on the different roles of audiometrists and audiologists and the range of services available.
- Professional Development: Support career stability and growth opportunities for hearing professionals to maintain the sector’s integrity.
- Simplified Access: Streamline the process for consumers to access hearing services and navigate the system.
- Cultural Competence: Enhance provider training to better meet the needs of diverse communities, including Indigenous Australians and the Deaf community.
Challenges and Opportunities
Implementing these reforms will not be without challenges. The hearing services industry in Australia is a complex ecosystem involving multiple stakeholders, each with their own interests and perspectives. The views of our constituents are that the current self-regulating model is not up to the task.
As one survey respondent noted, “There’s a lot of money in hearing aids, and some players in the industry might not want to see that change.”
However, support for regulation from consumers and ethical providers presents a unique opportunity for positive change. By aligning the interests of those seeking and delivering care, there’s potential to create a more transparent, effective, and trusted hearing services sector.
On the Threshold of Meaningful Change
The current self-regulation system for audiologists and audiometrists in Australia reveals a complex and potentially problematic landscape of professional oversight.
We have concluded from the Deafness Forum Australia survey that there is an urgent need for reform in the country’s hearing services. As the population ages and the prevalence of hearing issues increases, addressing these systemic problems becomes more critical.
The path forward will require collaboration between government bodies, industry stakeholders, and consumer advocates.
Read the complete survey report: use the form here to request your copy of the report.

Feb 2025: It’s important for healthcare professionals to use accurate titles that reflect their qualifications and training.
In this editorial piece, Deafness Forum Australia shares its opinion on the importance of clearer distinctions between audiometrists and audiologists.
Members of the community may encounter both audiometrists and audiologists when they seek hearing assistance, but would they know the difference?
There appears to be confusion among consumers about the roles of audiometrists and audiologists, with some expressing uncertainty about the expertise each profession possesses. This points to a need for better public education about professional roles and where the current system could be enhanced.
Terms like ‘audiology professionals’, ‘audiology profession’ and ‘audiology clinics’, are often used in advertising which can contribute to consumer confusion. The use of unclear terminology makes it harder to understand the qualifications of different service providers.
We believe that establishing a consistent national standard for both audiologists and audiometrists, supported by strong governance structures and evidence-based data, could help ensure that consumers receive accurate information. This approach aims to empower individuals to make informed decisions about their hearing health care. We are committed to collaborating with all stakeholders to ensure that these improvements are made together, with them, and not for them.
Differences between audiometrists and audiometrists
Audiometrists
are involved in conducting hearing assessments, managing hearing devices, and providing advice on rehabilitation programs primarily with adult clients. They usually hold a Diploma in Audiometry which involves two years of study at TAFE followed by a formal supervision program through a recognised employer. Some audiometrists may also then complete a Bachelor of Audiometry.
Audiologists
are university trained health professionals, with the entry level educational requirement being a postgraduate two-year Master of Audiology degree. They work in a range of settings: hospitals, government hearing clinics, private practice, academia and research, schools for individuals with impaired hearing, and hearing instrument manufacturers. They are the main provider of services relating to hearing and balance disorders including diagnosis, non-medical/surgical treatments and rehabilitation.
It has been difficult to determine how many practitioners there are in Australia. There were 2,492 accredited audiologists in 2021, according to A Review of the Literature Relating to the Hearing Health Care Workforce in Australia (2021): anecdotally, we have heard of figures as high as 3,500 and greater. The same report notes 665 audiometrists who were members of the Australian College of Audiology and the former Hearing Aid Audiology Society of Australia. The report does not attempt to estimate audiometrists who were not members of the professional bodies.
National Survey
To capture the experiences of receiving or delivering hearing services in Australia, Deafness Forum Australia’s constituents (consumers primarily, but also service providers) were invited to complete an in-depth survey. You can download the survey report here.
Consumers’ comments illustrate their views on the differences between audiometry and audiology providers:
- I was not aware of audiometrists
- It would be helpful to clearly explain the roles of audiologists and audiometrists to the public
- Clear identification of healthcare professionals is important for transparency.
Survey respondents who were providers of hearing care services (mostly audiologists, we conclude), including business owners, raised potential concerns about the delivery of hearing services by those who are not audiologists. These are comments from providers:
- It’s important for healthcare professionals to use accurate titles that reflect their qualifications and training. Clear titles help ensure transparency and trust with the public.
- Patients with complex conditions like tinnitus benefit from specialised care. Clear referral guidelines can help ensure they receive the appropriate level of expertise.
- Defining the scope of practice for audiologists and audiometrists can help clarify roles and responsibilities. Additionally, providing pathways for professional development can support career advancement and improve patient care.
Our survey on hearing services has provided valuable insights into the industry’s current state, but it also has a limitation: the underrepresentation of audiometrists. We encourage audiometrists to participate in our survey to gather more responses and ensure that their perspectives are heard. We have invited their professional body to share our survey and contribute editorial to One in Six to outline its views and aspirations for its members. We would also like to hear from employers. This collaborative approach will help the community better understand the needs and challenges faced by audiometrists.
Clarifying Roles for Better Consumer Outcomes
The Department of Employment and Workplace Relations is conducting an Audiometry Qualification Review.
Deafness Forum Australia supports the continued growth and development of the audiometry profession. We believe in quality education that meets an agreed national standard for audiometrists’ specialised skills in assessing adults, performing basic hearing tests, battery and hearing aid fittings.
We believe each consumer should receive person-centred care tailored to their individual needs. In our view, it’s important for audiometrists and audiologists to collaborate as a team, ensuring clear referral pathways are in place, ideally guided by a consistent, evidence-based national standard.
While existing processes are in place, we see an opportunity to strengthen them by uniting under a single national standard. We think this approach could facilitate smoother transitions in care, allowing audiologists to build on the work provided by audiometrists, and potentially enhance service delivery. We support a clear separation of roles between audiologists and audiometrists. We believe collaboration between the two professions should be coordinated and transparent with a clear structure in place to ultimately ensuring seamless care for consumers.
Can Mandatory Regulation of All Audiologists and Audiometrists Solve this Dilemma?
The debate over regulating audiologists and audiometrists in Australia is complex and multifaceted. Currently, the profession is largely self-regulated, with professional bodies Audiology Australia and the Australian College of Audiology representing membership of their bodies as a form of regulation. However, other stakeholders, including Independent Audiologists Australia and Deafness Forum Australia, strongly support mandatory registration under the Australian Health Practitioner Regulation Agency.
Challenges and Opportunities
The hearing services industry in Australia is a complex ecosystem involving multiple stakeholders, each with their own interests and perspectives. Some of our constituents feel that the current self-regulating model may face challenges in ensuring consistent quality across the industry.
One respondent in our national survey (you can download the report here) expressed concerns about the potential influence of financial interests in the hearing services industry stating:
“There’s a lot of money in hearing aids, and some players in the industry might not want to see that change…”
While this reflects one perspective, we recognise it may be one of several factors that require further exploration to ensure clarity and consistency within the system, ultimately ensuring that consumers receive the care they need.
The opportunity for positive change is here. Our survey suggests growing support for independent, national regulation from consumers and providers presenting a unique chance to strengthen and improve our hearing health services system. Now is the time to take meaningful steps toward enhancing the system and ensuring better outcomes for everyone.
- Here is the survey for hearing professionals to complete
- This one is for consumers of hearing services to complete

DEC 2024: Australia’s State and Territory Health Ministers are considering options for regulating the audiology profession
Health Ministers throughout Australia commissioned an investigation to assess future options for regulating the audiology profession.
Targeted consultations (Dec and Jan) are underway to inform research and analysis.
A consultation paper was created to guide and inform this stakeholder consultation. Here is the paper: Queensland Health | Consultation Paper 2 | Audiology Decision RIS
Deafness Forum supports the most comprehensive and safest model option, national registration under the National Registration and Accreditation Scheme administered by the Australian Health Practitioner Regulation Agency. If you have views that support our position to include in our submission, contact Hayley Stone, our National Director of Policy & Advocacy, for a confidential chat.
Protecting the Public from Unsafe Practice is our Priority
Comprehensive knowledge and expertise in managing the complex nature of deafness and hearing loss is critical across all hearing health practitioners. The public is at risk if other vulnerabilities are not recognised and addressed as part of hearing health services.
Hearing loss and deafness are often identified at vulnerable points in life, such as when a child is newly born or during advanced age, when cognitive decline may be present. Hearing loss is often a symptom of a broader health condition and can coexist with other disabilities.
Deafness Forum Australia is committed to supporting the registration of audiologists and audiometrists in Australia under the National Registration and Accreditation Scheme, emphasising the benefits it would bring to public safety.
Supporting Audiologists and Audiometrists
Deafness Forum Australia values the expertise and dedication of audiology and audiometry professionals. We aim to further support these practitioners by advocating for a structured registration process that ensures ongoing quality and recognition for qualified practitioners.
Regulation presents an opportunity to strengthen trust between individual consumers and their chosen audiology professionals. Building this trust can enhance the support for individuals experiencing hearing loss and deafness, ensuring they receive the necessary care and assistance they need.
Non-zero-sum gain
The challenge in making a case for registering audiologists and audiometrists in Australia under the National Registration and Accreditation Scheme is explaining that it is not a competitive, win-lose scenario.
We believe that all parties will benefit – the community, the profession, device retailers and governments. It’s a win-win for Australia.
Ensuring Consumer Safety: Protected Titles Are Important
Currently, audiologists are self-regulated, meaning their title is not legally protected, which could leave consumers more vulnerable to unqualified practitioners.
Implementing registration would legally protect the use of practitioner titles such as “audiologist” or “audiometrist”, ensuring that only those who meet mandatory qualifications and standards can use them.
In Australia, titles like “physiotherapist” and “doctor” are legally protected under the National Registration and Accreditation Scheme (NRAS), managed by AHPRA*, meaning only qualified professionals can use these titles. Without similar protections for titles like “audiologist” or “audiometrist”, there is a risk that someone could use these titles without the necessary qualifications, which could harm consumer safety. * The Australian Health Practitioner Regulation Agency, aka AHPRA, protects the public by regulating Australia’s registered health practitioners.
AHPRA’s system includes a national register for protected titles, allowing consumers to verify credentials and report unregistered practitioners. This also allows for a national consistent complaint pathway. While Australian Consumer Law offers some protection against misleading claims, AHPRA’s registration system provides stronger safeguards by ensuring professionals meet national standards and are monitored for ongoing competence.
State healthcare complaint mechanisms currently offer limited safeguards. A code of conduct exists for all unregistered healthcare practitioners, but being state specific, suspended individuals could move interstate and continue to practice.
Self-Regulation: Limited Scope
Because audiology is a self-regulated profession, qualified audiometrists and audiologists may opt into being regulated through membership of a professional body. Professional bodies will accredit their members if they complete prescribed and ongoing education and work hours, but there is no legal requirement to be a member of a professional body, and accreditation is primarily recognised for public and private health funding purposes.
The professional bodies can only investigate complaints about their members. If misconduct is proven, the professional bodies can only counsel and train them, and if needed, terminate their membership. Professional bodies can’t prevent non-members or those who commit misconduct from delivering hearing services; and they can’t influence anyone who is not a member.
The Right to Complain can be a Complex Pathway
The process of making a complaint can be complex and time consuming and therefore, a disincentive to raising concerns. Determining which complaint mechanism to use requires understanding of various complaint authorities, and those who start a complaint process with one authority may be told to take their complaint elsewhere. Complaints against a business require a complaint to Fair Trading (different names apply in different states) or The Australian Competition and Consumer Commission (ACCC).
The registration of audiologists and audiometrists in Australia under the National Registration and Accreditation Scheme could simplify the complaint process for consumers. With a centralised registry, such as AHPRA’s, consumers can more easily verify credentials and navigate the complaint system, allowing for a more straightforward and effective way to address grievances.
Mandatory Registration for Many Healthcare Professionals in Australia
Registered healthcare professionals in Australia are regulated under the National Registration and Accreditation Scheme (NRAS). Only professionals listed on that register are allowed, by law, to use
the title of that profession. For example, anyone who uses the title optometrists in Australia must, by law, be on the national register.
Registration of health professions under the NRAS offers assurance to the public that the practitioner has met consistent national standards. Numerous health professions are already regulated this way, including occupational therapy, optometry, osteopathy, pharmacy, physiotherapy, and podiatry as well as medical doctors and nurses.
National Registration and Accreditation requires professionals to hold recognised qualifications and renew their registration annually and requires them to participate in ongoing professional education.
The public can search for registered healthcare professionals through the Australian Healthcare Practitioner Regulation Agency website.
Complaints against registered professionals are investigated by the relevant appointed board. Mandatory registration for health practitioners ensures standards through meaningful penalties for unprofessional conduct. Penalties can include suspension or deregistration, meaning that the person cannot practice that profession any longer anywhere in Australia.
Deafness Forum Australia’s Position
Protecting the public from unprofessional practice is a priority for Deafness Forum Australia.
Deafness Forum Australia supports the registration of audiologists and audiometrists under the National Registration and Accreditation Scheme, emphasising the benefits it would bring to public safety.
We believe that registration would enable the public to trust that they will receive services from suitably qualified professionals, registered with a national body and to have a transparent and simplified complaints pathway when they do not.
Benefits All Australians
We want consumers to trust audiology and audiometry services in the same way they trust others who provide their healthcare, such as general practitioners, nurses, or optometrists.
Mandatory professional registration would mean that the public could trust the titles audiologist and audiometrist, so that anyone calling themselves an audiologist must have university qualifications in audiology. Audiologists achieve a Masters’ level qualification to provide their primary care role.
Audiometrists complete a range of certifications, including to diploma level, and conduct hearing tests across a range of settings.
Currently, there is the potential for public and health professional confusion about the expected role of the two professions.
Without registration and title protection, there is no mechanism to address this. (From Unleashing the Potential of our Health Workforce – Scope of Practice Review Final Report, Oct 2024)
Mandatory registration will offer more accessible information about each registered audiologist or audiometrist via an online search of a single government-maintained website.
A simplified complaints pathway that applies to all registered professionals will be open to consumers.
Anecdotal evidence suggests practitioners would value registration and hope to affirm their professional status through the same mechanism that recognises their colleagues in other healthcare professions.
Being registered will provide audiologists and audiometrists with formal acknowledgment of their qualifications and competence. We believe that audiologists and audiometrists will gain professional credibility and recognition from other healthcare professionals as fellow registered practitioners.
Deafness Forum Australia is committed to bringing the consumer voice to the decision-making. Your lived experience as consumers, how you have engaged with audiologists, audiometrists or others in the hearing services in hospitals, school, private, commercial or government settings, is important and deserves attention.

NOV 2024: The Untimely Demise of the Telecoil?
There are concerning signs in Australia that hearing device manufacturers are prematurely phasing out the Telecoil function, which provides crucial connectivity to public Hearing Loops.
Forced obsolescence is occurring despite the continued relevance and widespread use of Telecoil technology in many countries.
Hearing Loops connected to Telecoils in hearing devices dramatically increase the intelligibility of what is being said over public address systems and other large-area broadcasts.
This is because the “speech to noise ratio” that’s so important in hearing and understanding conversation is heavily weighted to speech as opposed to noise.
User-friendly hearing loops are common in the United Kingdom, much of Western Europe, and Australasia. In the United States, hearing loops are increasingly found in theatres, places of worship, and other places where people with hearing loss can expect to have difficulty hearing. The pace of loop installation has not slackened.
Australia is In The Loop
In Australia’s transportation sector, hearing loops are part of the Agil Passenger Information System in the new six-car passenger trains planned for the state of Queensland.
Melbourne is getting 25 new ultra-modern trains called X’Trapolis 2.0, which will cost $1 billion and feature hearing loops in the passenger cars.
A significant portion of people with hearing loss have telecoil-equipped hearing aids that give them access to hearing loops like those described above. It could be five and more years before the majority of those hearing aids have been replaced with hearing aids capable of connecting to emerging assistive listening systems using Bluetooth’s Auracast broadcast audio technology.
Consequently, it’s expected that the current pace in the installation of hearing loops – and the related need for hearing devices equipped with a Telecoil – will not slacken for a good many years.
From Hearing Aid Telecoil and Loop Update 2024.
Don’t Throw Baby Out With the Bathwater
The European Federation of Hard of Hearing People (EFHOH) emphasises the need for a balanced approach that values both emerging and existing technologies to ensure uninterrupted communication accessibility. EFHOH advocates for the continued inclusion of telecoils in hearing aids and cochlear implants for at least the next 10 to 15 years. This advocacy is grounded in the reality that it will take considerable time before newer technologies, such as Auracast transmitters, are not only widely available in public buildings but also fully integrated into all hearing aids, ensuring comprehensive accessibility.
EFHOH’s stance is supported by experiences and recommendations discussed in international forums, like the Budapest Declaration during the 2022 World Congress of the International Federation of Hard of Hearing People, which highlighted the necessity of telecoils coexisting with new technologies like Auracast™.
EFHOH reminds Audiologists and Audiometrists about their role as frontline hearing care professionals: they are gatekeepers of information and are responsible for informing their clients about Telecoils and Bluetooth features in their devices. Both features should be demonstrated for greater adoption.
Technological Integration and Consumer Impact
While Auracast™ promises enhanced flexibility in the future by allowing users to stream audio from multiple sources, the accessibility and reliability of telecoils in public spaces remain unmatched. The transition to new technologies faces technological and regulatory hurdles that could delay widespread adoption. Therefore, ensuring that hearing aids and cochlear implants continue to feature telecoils is essential for uninterrupted access to established assistive listening systems.
Voices from the Field
We have often heard that hearing loops “are redundant” and have been overtaken by newer technologies. Telecoils and hearing loop systems might be old technology, but so is the wheel.
And like the wheel, they continue to offer a quality, fit-for-purpose solution.
New and emerging technologies will undoubtedly supersede them in time, but are we there yet?
Better Hearing Australia advocates for the ongoing relevance of telecoils, suggesting that while new technologies are welcome, the real-world effectiveness and user-friendliness of existing systems like hearing loops must be considered. They stress the importance of these systems in delivering immediate and reliable solutions without the need for wearers to disclose their hearing loss or manage additional devices. Additionally, there is concern about user acceptance among older people who might prefer the familiarity and straightforward operation of Telecoil-based systems.
Hybrid Solutions for Accessible Listening
Recognising the slow adoption rate of Auracast™ among current hearing aid models and the continued relevance of telecoils, Univox (a major overseas manufacturer of hearing augmentation products) recommends a pragmatic approach: a hybrid system combining both Auracast™ and induction loops. This ensures backward compatibility and future-proofing, enabling venues to accommodate both traditional telecoil users and those adopting new technologies. Such an approach not only broadens accessibility but also aligns with inclusive design principles, ensuring that technological advancements do not exclude those dependent on existing solutions. It emphasises the importance of maintaining the well-functioning hearing loop systems, advocating against abandoning proven technologies.
The Role of Major Buyers
While it’s challenging to influence large international manufacturers to retain telecoils, major buyers such as the Australian Government play a crucial role.
Government programs must not inadvertently hasten an untimely end to public hearing accessibility. By mandating the inclusion of hybrid systems in their procurement contracts, the National Disability Insurance Scheme and the Hearing Services Program can ensure that all hearing devices they fund are equipped with telecoils for the foreseeable future. This will safeguard continued access to hearing augmentation systems that many rely on daily.
SEP 2024: Past Reviews, Future Vision: Discussion Paper Summary
In our discussion paper, “Past Reviews, Future Vision,” we explore how the Australian Government Hearing Services Program (the Program) has evolved over time.
We look at three key reviews from 2012, 2017, and 2020/21 to understand what actions have been taken, identify any gaps, and suggest improvements for better hearing health for all Australians.
Currently, one in six Australians experiences hearing loss, and this number is expected to rise to one in four by 2050. This makes it essential to provide high-quality support for everyone who needs it.
Our paper starts an important conversation about the challenges and opportunities within the Program. We propose a framework focusing on key areas like putting participants first, offering tailored support, addressing overall health needs, providing accessible information, and ensuring assistance for vulnerable groups. By collaborating with the community and stakeholder organisations, we aim to ensure that all Australians can access the hearing support they need at every stage of life.
As you read our paper, we invite you to think about what improvements could be made and how we can work together to enhance the Hearing Services Program for everyone. Together, we can create a more inclusive and effective program that helps all individuals thrive.
- Read the DeafnessForumAustralia Hearing Services Discussion Paper
- View our webinar launching the paper
- Read the Launch Webinar Transcript

June 2024: Australia’s State and Territory Health Ministers are considering options for regulating the audiology profession
Update, OCT 2024
“On 16 August 2024, the Ministerial Council considered the Audiology Decision RIS.
“Following this, Ministers have requested further work on implementation of audiology regulation under the National Registration and Accreditation Scheme, including targeted consultation to inform a final decision.
“The Queensland Health Project team will progress this additional work on behalf of the Health Workforce Taskforce with a planned update to the Ministerial Council in early 2025.”
Office of Minister for Health, Mental Health and
Ambulance Services and Minister for Women
Queensland Government.
Occupational therapists, optometrists, osteopaths, pharmacists, physiotherapists and podiatrists are among the 16 professions regulated by an independent regulatory body. Yet, audiologists regulate themselves via their own peak body.
We support action to ensure that the scope of service delivery performed by audiologists is aligned to nationally prescribed levels of knowledge, skills, and experience, and that professional qualifications mechanisms exist to manage underperforming audiologists, as well as those who engage in unethical business practices.
Deafness Forum Australia considers having a single organisation, independent of the profession, that has oversight or authority to investigate and consistently manage complaints and apply sanctions across the audiology profession to be essential to protect the community and enhance the reputation of the audiology profession.
Our Recommendation
Deafness Forum Australia strongly supports the registration of the audiology profession under the National Registration and Accreditation Scheme.
We recommend that it be expanded to cover national registration of both audiologists and audiometrists.
March 2024: First Nations Roundtable
Deafness Forum Australia hosted a roundtable meeting with a select group of influential stakeholders with a shared aim of helping to address the ear care and hearing health disparities in First Nations communities.
The Roundtable, in March 2024 in Canberra, was facilitated by Prof Kelvin Kong AM, an eminent ear, nose and throat surgeon and ardent social advocate. We discussed pivotal aspects of healthcare access and delivery, focusing on the challenges. From the Roundtable, an official communique was created: Meeting Communique – Addressing Aboriginal and Torres Strait Islander Hearing Healthcare MAR-2024
To augment the communique, we prepared a report that aligns the Roundtable outcomes with Closing The Gap Agreement priorities and the Roadmap for Hearing Health: Aligning Strategies with National Priorities – Roundtable Indigenous Hearing Healthcare MAR-2024.
Also in March, our national newsletter was a tribute to the talent, resilience and wisdom of Aboriginal Women in Hearing Healthcare and Advocacy. You can download and read this special edition of One in Six.

- Closing The Gap: Addressing the hearing health of Aboriginal and Torres Strait Islander Peoples in the criminal justice system.
Australia’s justice system remains ineffective in addressing the complex needs and vulnerabilities of Aboriginal and Torres Strait Islander peoples. We must stop the perpetual cycle that exists between childhood ear disease and the disproportionally higher rates of incarceration for this population. Read our report, Hearing Health of Aboriginal and Torres Strait Islander Peoples in the criminal justice system APR 2024.
- High Proportion of Indigenous Canberrans in Prison
Nearly a third of Canberra’s average prison population is Indigenous, despite Indigenous Canberrans constituting only 2% of the ACT population. The Australian Capital Territory is currently facing a significant challenge, with the highest rate of incarceration rates for Indigenous people in the nation compared to non-Indigenous residents. A critical yet often overlooked aspect of the plight of First Nation Australians in incarceration warrants attention: undiagnosed and untreated hearing loss. Read more on this topic here.

Navigating Barriers and Promoting Inclusivity
In producing this report, our primary aim was to highlight the pressing concern of inadequate hearing service access for people from culturally and linguistically diverse backgrounds.
We examined existing research and summarised the findings in accessible language. We hope that this paper will foster enhanced awareness of these issues, spark meaningful dialogue and further research and collaborations in the field. We offer clear recommendations to policymakers, hearing healthcare practitioners, and community program managers. Here is where you can read the report.
Disability Employment Centre of Excellence
Deafness Forum Australia provided its suggestions for the creation of a national Disability Employment Centre of Excellence.
This Centre, to be established by the Australian Government, aims to significantly improve employment opportunities for individuals with disabilities, addressing the persistent employment gap across Australia. Despite their eagerness and ability to work, people who are deaf or hard of hearing face higher unemployment rates than people without disability and can experience numerous employment barriers, including attitudinal, environmental, and systemic challenges. We’ve listed what we think should be the Centre’s goals. Read more here.
Hearing services provided through the National Disability Insurance Scheme and the way to improve them
When the Australian Government initially discussed its plans to transfer existing hearing services to the National Disability Insurance Scheme, we received assurances from both the NDIA and the Department of Health & Aged Care that service quality and timeliness would be maintained, with the goal of improvement.
They also assured us that the costs to the Commonwealth would not exceed the current expenses at that time. However, neither of these assurances have been fulfilled.
Given these circumstances, a service delivery model should be adopted that ensures easy access to high-quality and consistent hearing services at a reasonable cost to the government. Read our recommendations in a letter to the Review of the NDIS conducted by the Commonwealth Department of Prime Minister and Cabinet.
Attaining universal inclusion of all people who need the support of the NDIS
In a submission in 2023 to the Government review of the NDIS, we identified 9 key factors that if addressed, can dramatically improve the community’s trust in the NDIS.
Preventing hearing loss with Safe Listening Habits
Preventive health action is the key to achieving a healthier Australia by 2030. Avoidable hearing loss represents an enormous social and economic cost to Australia. Prevention is the most effective way to reduce hearing loss and tinnitus. Exposure to noise, whether prolonged or of short duration, is a major cause of approximately one-third of adult-onset hearing loss. And it is almost entirely avoidable. Read more about Preventable hearing loss. You can also read about Australia’s National Preventive Health Strategy 2021-2030 – it provides a high-level guide to preventive health actions.
Unaddressed hearing loss is a serious public health problem
Australians with good hearing health are better able to lead fulfilling and productive lives. People who have untreated hearing problems tend to have much higher general healthcare costs than those without hearing loss – as much as 50% more. Along with the distress experienced by individuals with hearing loss and the financial costs faced by families, hearing loss results in an annual cost to Australia’s economy of $30 billion dollars. Read more about Australia’s high levels of untreated hearing loss.
Crisis in Children’s cochlear implants in hospitals in two states
There are two state government investigations currently underway, but we feel that independent investigations may be necessary to earn community trust.
We will keep the community posted as we work through how we can constructively contribute to the investigation and systems improvements. The immediate priority is supporting the families and children, and if you go to the following web links you can read what we have recommended on their behalf.
- Cochlear implant crisis at Adelaide Children’s Hospital
- Two stood down as QLD health investigates cochlear crisis
Addressing the burden of hearing loss among vulnerable groups in the community
The objective of the Australian Government’s Hearing Services Program should be to ensure that vulnerable groups, those requiring specialised programs to address their hearing needs, and people on low income have access to high-quality hearing services at no cost or minimal cost. In order to do so, the eligibility of the Program should be extended to a broader group of vulnerable people:
1. People on a Health Care Card, or Low-Income Card
2. Seniors Health Care Card Holders
3. Children of refugees
4. People in the criminal justice system
5. People in Aged Care
Creation of a new eligibility category for Aged Care under the Community Service Obligations component of the Australian Government Hearing Services Program
Residents of aged care facilities are currently unable to access the hearing services they need under the Voucher Program component of the Hearing Services Program (HSP). These clients have complex needs and research has shown that residents in aged care require a different model of service delivery than is available through the Voucher Program.
Testing to detect noise-induced hearing loss in the workplace
The inability to hear can be a significant threat to a worker’s health and safety. Occupational hearing loss and deafness is a completely preventable injury. It is a serious injury that has a profound impact on an individual’s quality of life.
Two characteristics of noise-induced hearing loss have been thoroughly established. The amount of hearing loss increases with noise intensity, duration and exposure, such that more intense and longer-duration noise exposures cause more severe hearing loss.
Deafness Forum Australia, Unions NSW, The Australian Workers Union (NSW Branch), and affiliate unions believe it is important to test a worker’s hearing at the commencement of their career (within three months of the worker commencing work where hearing protection is required), to provide a baseline measurement as a reference for future audiometric test results. Once this is done, early identification of changes to hearing due to noise is the most effective way of assessing the effectiveness of any control measure in place and in turn preventing hearing loss, which can take place over a long period of time or can in some cases be instant. Follow-up testing should occur every two years. Testing should occur well into the work shift so that any temporary hearing loss can be picked up. More frequent audiometric testing may be needed if exposures are equal to or greater than 100dB(A).
Not only does early detection of noise-induced hearing loss through audiometric testing in preventing further hearing loss, it also assists in the medical and scientific study of hearing loss.
